Introduction:
Response assessment at day 100 post Autologous Stem Cell Transplant (ASCT) is associated with long-term relapsed free survival (RFS) and overall survival (OS) in multiple myeloma (MM). The International Myeloma Working Group (IMWG) are the preferred criteria to define best response to treatment and define relapse. In the last years, response assessment has incorporated minimal residual disease (MRD) status -associated with improved RFS and OS (Munshi et al); and PET/CT combined with clinical characteristics -also associated with favorable outcomes (Zamagni et al. NCT01910987; MMY3033). The 2016 IMWG MRD criteria, combined imaging (PET/CT) plus next-generation sequencing (NGS) MRD-negative to define complete response (CR). To our knowledge, there is limited data examining the correlation and prognostic value of MRD and FDG-PET/CT at day 100 post ASCT in MM. IN this study, we aimed to determine the prognostic valued of MRD by NGS combined with PET/CT in RFS and OS status after high dose chemotherapy and ASCT in MM.
Methods:
Patients who underwent ASCT for MM at Mayo Clinic Arizona and had MRD and PET/CT data were included in the study. Clinical data was obtained via retrospective chart review. Cytogenetic risk (CyR) was classified using the mSMART criteria . Disease and ASCT related characteristics were compared by MRD status. MRD was measured by NGS on bone marrow aspirates using the previosly validated clonoSEQ ® Assay (Adaptive Biotechnologies Corporation, Seattle, USA) tracking the IgH, IgK and IgL rearrangements at a minimum sensitivity level of 10-5. MRD was defined by residual clonal cells per million nucleated cells as: negative= 0, borderline= 1-5, positive >5. PET/CT scans were performed locally at baseline and at day 100. Comparisons were performed using the chi-square test for categorical variables, Wilcoxon rank-sum test for continuos variables, McNemar's test and Cohens's Kappa for agreement measures.
Results:
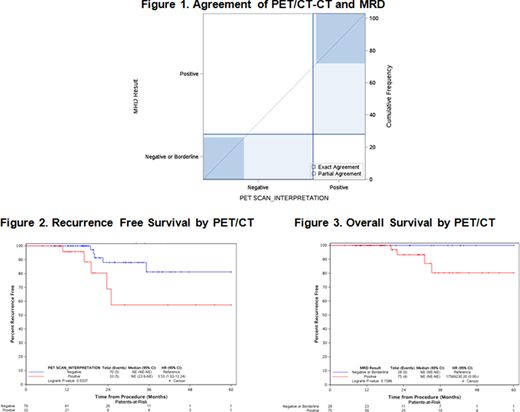
A total of 103 patients had matched MRD and PET/CT assessment around day 100 (+/-9 days) and were included in the analysis. Median age at diagnosis was 62 years (range, 54-66 years), 71 patients (68.9%) were men. CyR was standard risk in 49 (47.6%), high-risk in 39 (37.9%) and unknown in 15 (14.6%) patients. Most 75 (72.8%) patients were MRD positive, 16 (15.5%) were MRD negative, and 12 (11.7%) borderline. The median main MRD clone detected was 64 (range 0-91,874). 70 patients (68%) and 33 (32%) had a negative and positive PET/CT respectively. The median follow-up time was 18 months (range, 13-31 months). At the time of data analysis, 10 patients (9.7%) had relapsed and only 4 (3.9%) had died. There was a high-correlation between MRD status and PET/CT, 31 patients (93.9%) with positive PET/CT were also MRD positive (p=0.0027). There were no statistical differences between PET/CT and CyR (p=0.95). We analyzed the correlation using the FREQ procedure (McNemars's test); there was a strong association between positive PET/CT and positive MRD in 31/33 patients (93.9%, high sensitivity), and low association for negative PET/CT the negative/borderline MRD in 26/70 (37.1%, low specificity; p<0.001). The agreement measure between the PET/CT and MRD using negative/borderline combined had a kappa of 0.23 (95% CI 0.11, 0.35) indicating a fair agreement beyond chance (Figure 1). PET/CT-CT was a statistically significant predictor of worse RFS (HR 3.53, 95%CI: 1.02-12.24, p<0.0337) and OS (HR 11.38, 95%CI: 1.18-109.56, p<0.0078) (Figure 2-3, respectively). MRD was not predictive of neither RFS (HR 1.72, 95%CI: 0.36-8.14, p<0.49) or OS (p<0.16).
Conclusions:
In conclusion, we demonstrate that the combination of MRD by NGS (clonoSEQ ®) and PET/CT at day 100 are complementary and have a high sensitivity (true positive rate) and fair correlation of agreement but low specificity (true negative rate). PET/CT was the best most sensitive technique to prognosticate RFS and OS. We did not find prognostic correlation of MRD with RFS and OS. However, our findings might be confounded by the low risk of relapse and death, a longer follow-up may demonstrate clinically important differences. Our results add evidence that MRD plus PET/CT improve the definition of CR in MM patients post ASCT. Prospective studies are needed to elucidate the optimal timing and role of combined MRD, PET/CT with other prognostic markers of clinical outcomes.
Larsen:Takeda: Honoraria, Membership on an entity's Board of Directors or advisory committees; Janssen Oncology: Honoraria, Membership on an entity's Board of Directors or advisory committees. Fonseca:Juno: Consultancy; Kite: Consultancy; Aduro: Consultancy; OncoTracker: Consultancy, Membership on an entity's Board of Directors or advisory committees; Merck: Consultancy; Bayer: Consultancy; Janssen: Consultancy; Takeda: Consultancy; Novartis: Consultancy; Pharmacyclics: Consultancy; Sanofi: Consultancy; Oncopeptides: Consultancy; GSK: Consultancy; AbbVie: Consultancy; Adaptive Biotechnologies: Membership on an entity's Board of Directors or advisory committees; Amgen: Consultancy; BMS: Consultancy; Celgene: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal